What is a tooth abscess?
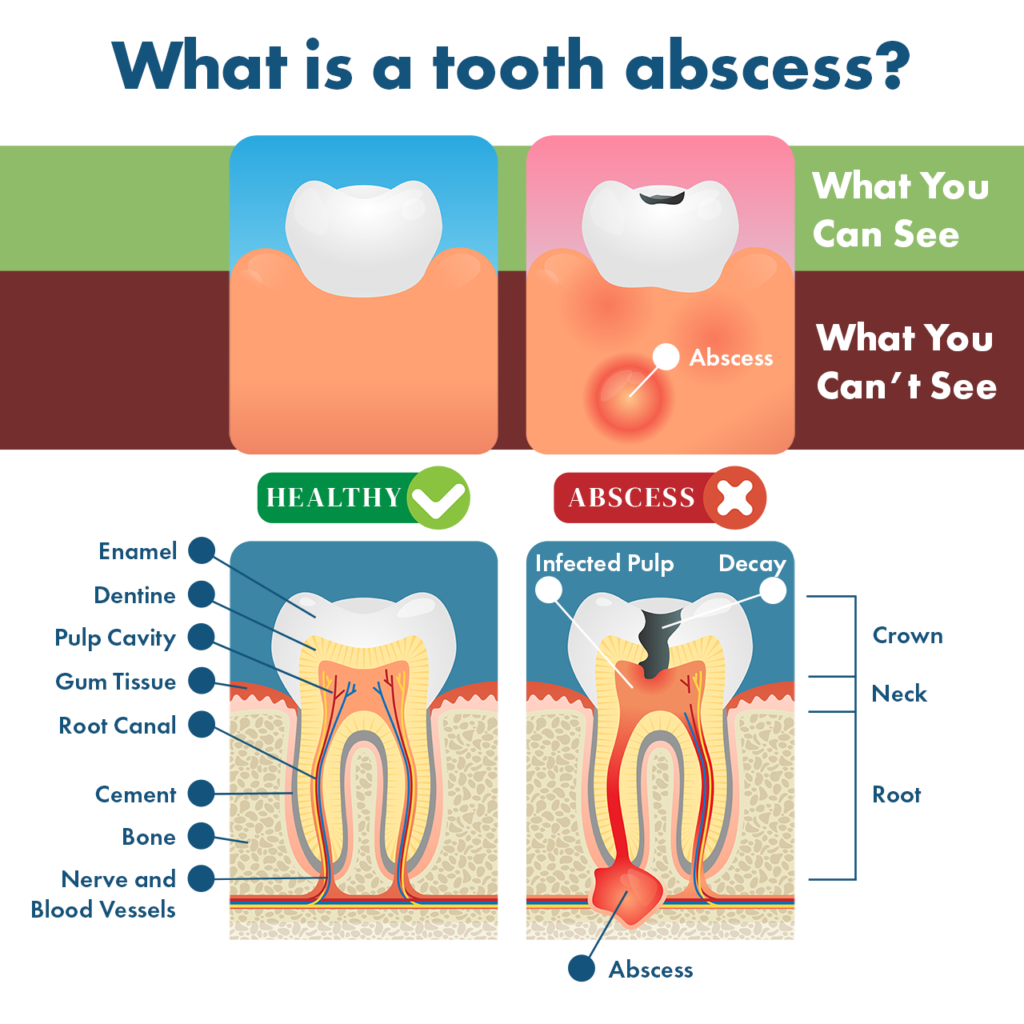
A tooth abscess is a pus pocket beneath the root of the tooth caused by a bacterial infection.
Usually, tooth abscesses are a result of untreated cavities, failed dental work, or an injury.
An abscessed tooth will cause a significant amount of pain in your gums, teeth, and sometimes radiating out to your ear and/or neck.
A tooth abscess is also referred to as a periapical abscess, while a periodontal abscess (gum abscess) develops next to the tooth root in the gums. Tooth abscesses are sometimes referred to as jawbone infections.
If you have a tooth abscess, you need to see your dentist, as this condition cannot be treated at home and is considered a dental emergency. Your dentist will drain the infection and correct the problem by either performing a tooth extraction or root canal.
Several homeopathic remedies may help reduce the pain of a tooth abscess while waiting to get to your dentist.
Get Dr. B’s Dental Health Tips
Free weekly dental health advice in your inbox, plus 10 Insider Secrets to Dental Care as a free download when you sign up

When to Call a Dentist
Call your dentist right away if you experience:
- Recurring throbbing pain in your teeth
- Pain that increases when you lie down
- Pain in your teeth or gums that interferes with daily activities such as working, eating, or sleeping
- Pain that refers to other parts of your jaw or other teeth (this will always happen on the same side of your mouth as the infected tooth)
Is a tooth abscess an emergency? Yes, a tooth abscess is a dental emergency that requires immediate care from a dentist.
Somewhere between 1-2 million ER visits in the US each year are for dental pain, and over 37% of these are due to tooth abscesses. However, a dentist is the best specialist to treat a tooth abscess, as they are trained and ready to address your exact problem, unlike an emergency room.
What do I do if I have a tooth abscess while pregnant? If you suspect a tooth abscess during pregnancy, call your dentist immediately. He or she will probably avoid an x-ray but will opt for treatment as quickly as possible to prevent pregnancy or birth complications.
The most painful part of treating an abscessed tooth is getting yourself to the dentist. But the dentist is exactly where you need to be — as soon as possible — to get rid of the pain and the underlying infection causing it.
If you do need to go to the emergency room for pain, they will probably prescribe antibiotics and anti-inflammatory painkillers and refer you to a dentist.
Dental Abscess Types
There are 3 types of dental abscess:
- Periapical abscess: Also known as a tooth abscess, a periapical abscess is a pocket of pus from bacterial infection at the tip (apex) of a tooth root.
- Periodontal abscess: Periodontal abscess, or gum abscess, starts in a periodontal pocket between the teeth and gums. This may eventually spread to the tooth and/or the periodontal ligament as a result of advanced periodontal disease. Gum abscess includes two sub-classifications:
- Gingival abscess: Gingival abscess is a type of gum abscess that has not spread to or damaged the tooth or periodontal ligament. This is more likely in early gum disease.
- Pericoronal abscess: A pericoronal abscess is also a gum abscess that affects the gums and other soft tissue around the crown of a tooth.
- Combined periodontal-endodontic abscess: This occurs when a periapical abscess and periodontal abscess combine together.
The information below refers specifically to a periapical/tooth abscess.
Symptoms
Tooth abscess pain around the tooth or in the gums is the most common and obvious symptom of a periapical abscess.
What does an abscessed tooth feel like? Usually, an abscessed tooth causes throbbing pain that begins suddenly and worsens over time.
Although the pain seems to come out of nowhere, a tooth abscess has likely been in the making for years. A tooth abscess may be asymptomatic for years before causing a toothache.
Symptoms of a tooth abscess include:
- Throbbing pain in the teeth and/or gums
- Pain radiating to the neck, ear, or jaw
- Painful chewing or biting
- Swollen upper or lower jaw
- Swollen lymph nodes in the neck or under your jaw
- Redness or swelling of the face
- Severe, lingering tooth sensitivity to hot and cold
- Trismus (“lockjaw”)
- Headache
- Nausea
- Fever
- Bad breath
- Bitter or bad taste in the mouth (often described as salty)
- A draining sore on the gum
- An ache in the bone around your affected tooth
- General malaise (feeling sick)
- Cutaneous dental sinus tract (an infectious lesion inside or outside the sinuses or face)
- Cellulitis (bacterial skin infection) — may occur with or without other symptoms
Diagnosis
How does your dentist diagnose a tooth abscess? Your dentist will perform a physical assessment of your face, lymph nodes, and the inside of your mouth, as well as an intraoral x-ray and/or cone-beam CT (CBCT), to diagnose a tooth abscess. He or she will tap on (palpate) your teeth, as an infected tooth is usually sensitive to touch.
Common external signs of a tooth abscess include red, swollen gums and visible tooth decay.
He or she will perform “differential diagnosis” with your symptoms and imaging results to consider related conditions that could otherwise cause your symptoms.
Is it an abscess, or something else? Only your dentist can diagnose a tooth abscess with certainty. Tooth abscess pain is severe, but it’s not the only cause of severe dental pain.
Can my doctor or dentist misdiagnose a tooth abscess? It is possible for your primary care physician to misdiagnose a tooth abscess as something else. Sometimes, the opposite happens and a tooth abscess is misdiagnosed even though the underlying condition is different.
One reason this happens is that abscess infection spreads to other parts of the body if it’s not addressed. Referred symptoms from your infected tooth can make a diagnosis more difficult.
Conditions that present symptoms similar to a tooth abscess include:
- Oral cancer
- Scrofula (a cause of tuberculosis)
- Actinomycosis (a rare infectious disease)
- Cat scratch disease (Bartonella infection)
- Ewing’s sarcoma (a rare type of malignant bone tumor)
- Cemento-osseous dysplasia (a jaw condition in which connective tissue and abnormal bone fuse with normal bone tissue; looks like tooth abscess on x-ray)
- Non-Hodgkin’s lymphoma of the gingiva (a rare form of oral non-Hodgkin’s lymphoma)
Causes & Risk Factors
The most common causes of tooth abscess are untreated cavities (tooth decay), injury to the tooth, or failed dental work.
An abscess after dental work is much less common than one caused by untreated cavities or injuries.
Risk factors for tooth decay/cavities include:
- Diet high in sugar and other refined carbohydrates
- Mouth breathing/dry mouth
- Antibacterial dental hygiene products that disrupt the oral microbiome
- Lack of vital nutrients for healthy teeth, such as vitamin K2 and D3
- Illicit drug use, especially methamphetamines
- Smoking
- Poor dental hygiene
- Trauma to the teeth and/or face
An untreated cavity or crack in your teeth can “open the door” for bacteria to enter your dental pulp, which is in the center of your tooth. The dental pulp contains everything vital to the “life” of your tooth, such as blood vessels and nerves.
When bacteria get into the pulp, they cause swelling, inflammation, and pus, a condition known as “pulpitis.”
At first, when caused by infection, pulpitis is reversible (though with failed dental work or injuries, the pulp may be irreversibly inflamed almost immediately).
Eventually, pressure builds up, which is why you feel throbbing or sharp pain. This is known as “irreversible pulpitis,” and at this point, an abscess has formed that must be drained.
When the abscess is drained, the pain will dissipate almost immediately. However, pain relief does not mean that you’re free and clear. The infection is still there and must be addressed.
Treatments
Your dentist may prescribe antibiotics to reduce the infection in a tooth abscess and/or anti-inflammatory painkillers. Both of these treatments will help reduce your pain levels, but they are only temporary treatments.
There are only two tooth abscess treatments that will cure the underlying infection: root canal or tooth extraction followed by a dental implant.
Can a tooth abscess go away on its own? No, a tooth abscess can not go away on its own. There are no holistic treatments that can reverse an abscess once it has developed.
A gum abscess can rupture, which briefly relieves pain and may fool the patient into thinking the abscess has gone away. However, a periapical/tooth abscess cannot rupture.
Let’s take a look at the potential treatments your dentist may prescribe.
1. Antibiotics
At one time, antibiotics were the first-line treatment for dental abscesses to shrink the infection and address abscess-related toothache and facial pain. Today, they are used somewhat less often to reduce tooth abscess infection because of the concern of antibiotic resistance.
Four types of antibiotics are commonly prescribed for tooth abscess infection:
- Penicillin
- Macrolides (clarithromycin/Biaxin, azithromycin/Zithromax, fidaxomicin/Dificid, and erythromycin)
- Metronidazole (Flagyl)
- Clindamycin
For many bacterial infections, a doctor may wait to prescribe an antibiotic until they know which bacteria are causing the infection. This is not done for a tooth abscess, as test results take up to 14 days, by which time the infection can be fully corrected by dental treatment.
Dentists usually opt for penicillin first unless otherwise indicated for a specific patient as most infections of dental pulp are susceptible to this antibiotic strain.
Doctors will usually prescribe a 7-10 day course of antibiotics to shrink a tooth abscess.
Antibiotics will reduce the abscess infection and offer temporary relief. However, they do not cure an abscess; they are a short-term solution before extraction or root canal can be performed.
2. Pain Relief Medication
Non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen (Tylenol) are the most effective pain relievers for dental pain, including that caused by a tooth abscess.
Your dentist may prescribe you over-the-counter or prescription analgesics (painkillers) like:
- Ibuprofen (Advil)
- Naproxen (Aleve)
- Celecoxib (Celebrex)
- Aspirin (Motrin)
Opioids aren’t usually prescribed because they don’t work well for dental pain.
Like antibiotics, pain relief medications are prescribed only for short-term relief before a root canal or extraction can be performed.
3. Root Canal
Root canal treatment (endodontic therapy) is usually the treatment of choice for removing the infection that caused a tooth abscess.
A tooth abscess only forms when the pulp of your tooth is dead and cannot be saved due to the presence of irreversible pulpitis. Most dentists will attempt to treat your tooth abscess by first trying to save the existing tooth structure with a root canal.
Endodontic therapy (root canal) is usually preferred as a first option for correcting a dental abscess.
I look for several positive signs of root canal success before prescribing it to a patient:
- Negotiable canals (complex canals mean a much higher chance for re-infection)
- No calcified canals
- High chance of procedural success (no hidden fractures, etc.)
- A clear view of tooth root structure via cone-beam CT (CBCT)
After a root canal, your dentist will need to place a dental crown to protect your tooth from fracture. CBCT should be performed every 3 years to check for root canal failure.
Benefits:
- Retains your original tooth structure for no disruption to chewing or orthodontic growth
- Less invasive than extraction with a dental implant
- Less expensive than extraction with a dental implant
- Does not cause bone loss
- Heals within 1-2 days for fast relief
Risks:
- Not 100% “clean” and may leave behind bacteria that can lead to root canal failure and a further infection
- May not be possible with frail enamel or a very deep cavity
- Higher chance of tooth fracture because the tooth is no longer alive
- May cause systemic infection if a new infection occurs
- May fail due to underfilling, overfilling, or poor root canal procedure (requiring another root canal or tooth extraction)
Cost:
- Root Canal (by a dentist): $500-$1,500
- Root Canal (by an endodontist): $750-$2,250
- Dental Crown: $900-$1,700
Recovery Time: 1-2 days
Dental Visits Required: 2-3
4. Tooth Extraction
In a large number of cases, root canal therapy is either not possible or not advisable for tooth abscess treatment. If so, you’ll need to have the tooth extracted and plan for a dental implant.
Much of the time, your dentist will recommend a bone graft at the time of your extraction to prepare your jawbone for an implant.
Benefits:
- Unlike a root canal, 100% of the bacterial infection is completely removed
- No risk of tooth fracture
- Low risk of systemic infection from a second infection
- Does not need periodic follow-up to check for failure like root canal therapy
Risks:
- Without a dental implant, may lead to orthodontic shifting and issues with bite and possibly TMJ
- May result in a dry socket during recovery
- Associated with bone loss before the dental implant procedure
- More expensive than root canal therapy
- More invasive than root canal therapy
- More chance of failure depending on several factors, including which tooth is extracted
- Extraction or loss of teeth results in a slightly higher risk of heart attack than root canal therapy
Cost:
- Simple Extraction: $150-$200
- Surgical Extraction: $300-600
- Bone Graft: $200-$1,200 (up to $3,200 to use the patient’s own bone)
- Dental Implants: $500-$8,000 per tooth (averages between $3,000-$4,500 in the US)
Recovery Time:
- Simple Extraction: 1-2 days
- Surgical Extraction: 3-7 days
- Dental Implant: 2-3 days per procedure; the process takes 6-12 months to complete
Dental Visits Required: 2-3
Complications
Untreated dental abscesses have a number of very serious complications. They are rare or uncommon, but it’s important to address a possible tooth abscess so as to not put yourself at risk. At some point, your immune system may not be able to fight off the growing infection.
Complications of tooth abscesses include:
- Osteomyelitis: Infection of the alveolar bone or jawbone surrounding the affected tooth. This is most common in elderly or immunocompromised patients.
- Cellulitis: An infection of the skin that can infect soft tissue around an abscessed tooth.
- Parapharyngeal and/or peritonsillar infection: Abscesses that can form in the back of the mouth as infection from a tooth abscess spreads.
- Sepsis: Organ dysfunction due to a dysregulation in the body’s immune response after a severe infection. This is rare for dental infections — but it can happen — and is more common in patients hospitalized after a tooth abscess. In very rare cases, it may lead to death via multiorgan failure.
- Toxic shock syndrome (TSS): A form of septic shock caused by Staphylococcus or Streptococcus bacteria that can lead to sepsis. TSS may occur when abscessed teeth spread infection to other parts of the body
- Septic cavernous sinus thrombosis (CST): A rare complication of a dental infection that causes infection of the sinuses and possible facial palsy.
- Dentoalveolar abscess: Abscess of the orbit (bony cavities of the eye) resulting from a tooth abscess.
- Brain abscess: An abscess in the brain from the spread of tooth abscess infection. Symptoms of a tooth infection spreading to the brain include fever, stiff neck, chills, and changes in your vision or mental state.
- Ludwig’s angina and mediastinitis: Mediastinitis is inflammation of the chest cavity (mediastinum). A 2001 case report linked a patient’s tooth abscess and subsequent case of Ludwig’s angina (deep neck infection) to this inflammatory condition.
- Descending necrotizing mediastinitis: A life-threatening complication of oral or throat infections that spreads to the chest cavity. This is extremely rare but carries a very high mortality rate of 40%.
Home Remedies
How can you get rid of a tooth abscess without going to the dentist? You can’t — only a dentist can get rid of a tooth abscess.
However, there are several tooth abscess home remedies that may provide relief from your pain while you’re waiting on your appointment:
- Saltwater rinse
- Ibuprofen or other painkillers
- Clove oil
- Tea bags
- Cold compress
- Benzocaine
- Acupressure/acupuncture
- Wedge pillow/elevation
Just remember, homeopathic remedies can not cure your tooth abscess.
Prevention
To prevent a tooth abscess, you should practice good oral hygiene habits to reduce your risk of cavities. These include:
- Regular 6-month teeth cleanings/dental checkups to clear plaque and tartar buildup and check for new tooth decay or other issues
- Follow a diet to prevent and reverse cavities full of prebiotic (high-fiber) foods, healthy fats, high-quality animal products, fruits, vegetables, and nutrient-dense foods
- Brush your teeth twice each day and 45 minutes after a sugary, high-carb, or acidic meal or snack
- Use hydroxyapatite toothpaste (best option) or fluoride toothpaste to build strong enamel
- Floss at least once a day
- Scrape your tongue
- Use oral probiotics, especially if you have issues with recurring dental health problems
- Try oil pulling to reduce inflammation and balance the oral microbiome
- Replace your toothbrush or toothbrush head every 1-3 months and after you get sick
To reduce your risk of trauma to the teeth that can lead to an abscess:
- Always wear a mouthguard when you exercise or play sports
- Be very cautious in situations where falling is common, such as when walking on an icy sidewalk or hiking a difficult trail
- Avoid situations in which you might bump your face with a hard object (such as dancing closely at concerts or holding a wine glass close to your face during a cocktail party)
- Follow safe driving techniques and don’t sit too close to your steering wheel
Prognosis
When addressed by a dentist, a tooth abscess can be cured by a root canal or tooth extraction days to weeks after your pain begins. In general, the long-term outlook for a tooth abscess is very positive.
Treatments to cure a tooth abscess boast a healing time of just one week or less without complications — and the recovery involves far less pain than the infection.
Factors that lead to longer healing time after a dental abscess include:
- Presence of a fever
- Trismus (“lockjaw”)
- Abscesses in multiple spaces
- Abscess drainage
- Use of some antibiotics
However, if you do not seek treatment for a tooth abscess (or any dental abscess), very serious complications, including death, may occur. Your oral health will not be the only thing at stake, so don’t wait to call your dentist.
If you suspect a dental abscess, seek help immediately. The sooner you get things checked out by your dentist, the sooner you can get back to your life.
References
- Kloetzel, M. K., Huebner, C. E., & Milgrom, P. (2011). Referrals for dental care during pregnancy. The Journal of Midwifery & Women’s Health, 56(2), 110-117. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3074205/
- Roberts, G., Scully, C., & Shotts, R. (2000). Dental emergencies. Bmj, 321(7260), 559-562. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1118447/
- Nguyen, D. H., & Martin, J. T. (2008). Common dental infections in the primary care setting. American family physician, 77(6), 797-802. Full text: https://www.aafp.org/afp/2008/0315/p797.html
- Siqueira, J. F., & Rôças, I. N. (2013). Microbiology and treatment of acute apical abscesses. Clinical microbiology reviews, 26(2), 255-273. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3623375/
- Cantatore, J. L., Klein, P. A., & Lieblich, L. M. (2002). Cutaneous dental sinus tract, a common misdiagnosis: a case report and review of the literature. CUTIS-NEW YORK-, 70(5), 264-275. Full text: https://mdedge-files-live.s3.us-east-2.amazonaws.com/files/s3fs-public/Document/September-2017/070050264.pdf
- Statkievicz, C., Faverani, L. P., Gomes-Ferreira, P. H. S., Ramalho-Ferreira, G., & Garcia-Junior, I. R. (2016). Misdiagnosis of extensive maxillofacial infection and its relationship with periodontal problems and hyperglycemia. Case reports in dentistry, 2016. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4738737/
- ArunKumar, K. V., & Deepa, D. (2015). Migratory and misleading abscess of oro-facial region. Journal of Indian Society of Periodontology, 19(4), 470. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4555811/
- Keshani, F., Jahanshahi, G., Attar, B. M., Kalantari, M., Razavi, S. M., Hashemzade, Z., & Tavakoli, P. (2014). Ewing’s sarcoma in mandibular similar to dental abscess. Advanced biomedical research, 3. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3950843/
- Resnick, C. M., & Novelline, R. A. (2008). Cemento-osseous dysplasia, a radiological mimic of periapical dental abscess. Emergency radiology, 15(6), 367-374. Abstract: https://pubmed.ncbi.nlm.nih.gov/18726126/
- Martinelli-Kläy, C. P., Martinelli, C. R., Martinelli, C., Dias, J. B., Cheade, T. C., & Lombardi, T. (2009). Primary extranodal non-Hodgkin lymphoma of the gingiva initially misdiagnosed as dental abscess. Quintessence International, 40(10). Abstract: https://pubmed.ncbi.nlm.nih.gov/19898711/
- Shweta, S. (2013). Dental abscess: A microbiological review. Dental Research Journal, 10(5), 585. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3858730/
- Lin, L. M., Rosenberg, P. A., & Lin, J. (2005). Do procedural errors cause endodontic treatment failure?. The Journal of the American Dental Association, 136(2), 187-193. Abstract: https://jada.ada.org/article/S0002-8177(14)64408-1/abstract
- Akbar, I. (2015). Radiographic study of the problems and failures of endodontic treatment. International journal of health sciences, 9(2), 111. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4538887/
- Momin, M., Albright, T., Leikin, J., Miloro, M., & Markiewicz, M. R. (2018). Patient morbidity among residents extracting third molars: does experience matter?. Oral surgery, oral medicine, oral pathology and oral radiology, 125(5), 415-422. Abstract: https://pubmed.ncbi.nlm.nih.gov/29397341/
- Willershausen, B., Kasaj, A., Willershausen, I., Zahorka, D., Briseno, B., Blettner, M., … & Münzel, T. (2009). Association between chronic dental infection and acute myocardial infarction. Journal of endodontics, 35(5), 626-630. Abstract: https://pubmed.ncbi.nlm.nih.gov/19410072/
- Nezafati, S., Ghavimi, M. A., & Yavari, A. S. (2009). Localized osteomyelitis of the mandible secondary to dental treatment: report of a case. Journal of dental research, dental clinics, dental prospects, 3(2), 67. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3517289/
- Douglass, A. B., & Douglass, J. M. (2003). Common dental emergencies. American family physician, 67(3), 511-516. Full text: https://www.aafp.org/afp/2003/0201/p511.html
- el-Naaj, A., Krausz, A., Ardekian, L., & Peled, M. (2001). Parapharyngeal and peritonsillar infection following mandibular third molar extraction. Refu’at Ha-peh Veha-shinayim (1993), 18(3-4), 35-9. Abstract: https://pubmed.ncbi.nlm.nih.gov/11806045/
- Robertson, D., & Smith, A. J. (2009). The microbiology of the acute dental abscess. Journal of medical microbiology, 58(2), 155-162. Abstract: https://europepmc.org/article/med/19141730
- Fardy, C. H., Findlay, G., Owen, G., & Shortland, G. (1999). Toxic shock syndrome secondary to a dental abscess. International journal of oral and maxillofacial surgery, 28(1), 60-61. Abstract: https://pubmed.ncbi.nlm.nih.gov/10065654/
- Verma, R., Junewar, V., Singh, R. K., Ram, H., & Pal, U. S. (2013). Bilateral cavernous sinus thrombosis and facial palsy as complications of dental abscess. National journal of maxillofacial surgery, 4(2), 252. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3961908/
- Pellegrino, S. V. (1980). Extension of dental abscess to the orbit. The Journal of the American Dental Association, 100(6), 873-875. Abstract: https://pubmed.ncbi.nlm.nih.gov/6929838/
- Furst, I. M., Ersil, P., & Caminiti, M. (2001). A rare complication of tooth abscess-Ludwig’s angina and mediastinitis. JOURNAL-CANADIAN DENTAL ASSOCIATION, 67(6), 324-329. Full text: https://www.cda-adc.ca/jcda/vol-67/issue-6/324.html
- González-García, R., Risco-Rojas, R., Román-Romero, L., Moreno-García, C., & García, C. L. (2011). Descending necrotizing mediastinitis following dental extraction. Radiological features and surgical treatment considerations. Journal of Cranio-Maxillofacial Surgery, 39(5), 335-339. Abstract: https://pubmed.ncbi.nlm.nih.gov/21074449/
- Jarboui, S., Jerraya, H., Moussi, A., Ben, M. M., Marrakchi, M., Kaffel, N., … & Zaouche, A. (2009). Descending necrotizing mediastinitis of odontogenic origin. La Tunisie medicale, 87(11), 770. Abstract: https://pubmed.ncbi.nlm.nih.gov/20209836/
- Vargo, R. J., Warner, B. M., Potluri, A., & Prasad, J. L. (2017). Garlic burn of the oral mucosa: A case report and review of self-treatment chemical burns. The Journal of the American Dental Association, 148(10), 767-771. Abstract: https://pubmed.ncbi.nlm.nih.gov/28390650/
- Ottaviani, G., Costantinides, F., Perinetti, G., Luzzati, R., Contardo, L., Visintini, E., … & Biasotto, M. (2014). Epidemiology and variables involved in dental abscess: survey of dental emergency unit in Trieste. Oral diseases, 20(5), 499-504. Abstract: https://onlinelibrary.wiley.com/doi/abs/10.1111/odi.12164

 Oral Thrush: Home Remedies, Causes, Symptoms & More
Oral Thrush: Home Remedies, Causes, Symptoms & More