“Sleeping like a baby” is how we describe a perfect night’s sleep — restful and restorative. For children, sleep is a time of growth and brain development.
But many newborns and children aren’t sleeping well and, as a result, are missing out on that restorative sleep that lets them grow and develop to their genetic potentials.
Snoring, mouth breathing, and grinding and clenching the teeth are all signs of sleep-disordered breathing or obstructive sleep apnea in children.
How Does Mouth Breathing Hurt My Child?
While it may seem harmless, mouth breathing affects how your child develops, your child’s behavior and personality, as well as the adult that your child grows up to be.
Most healthcare professionals, including your doctor, might tell you not to worry about mouth breathing and insist that your child will “grow out of it.”
But the truth is, mouth breathing can have devastating effects on the development of the face and airway.
Get Dr. B’s Dental Health Tips
Free weekly dental health advice in your inbox, plus 10 Insider Secrets to Dental Care as a free download when you sign up

How Mouth Breathing Changes Facial and Oral Development
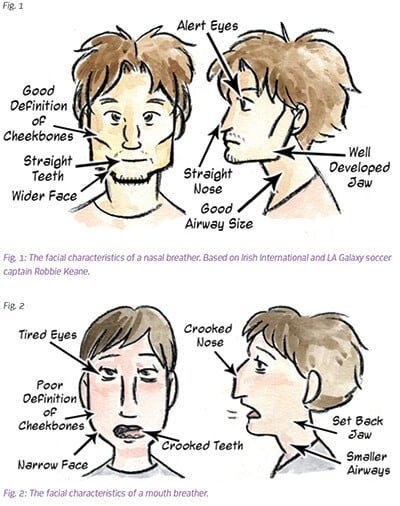
When nasal breathing is blocked, facial and dental development become abnormal.
In both human and animal studies, when nasal breathing is blocked, untreated mouth breathing leads to development of long, narrow faces with crooked teeth, receded jaw, and future TMD and headache issues.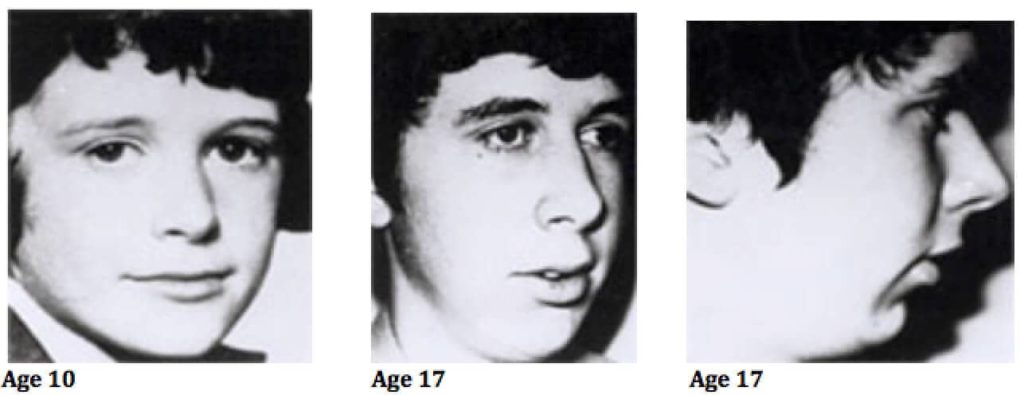
But it’s not just about looks. When the jaw and airway don’t fully develop, the airway can become easily obstructed during sleep.
During the complete muscle relaxation of deep stage sleep, the muscles around the airway also relax and collapse. The airway is a tight space, often made tighter by large tonsils and adenoids in both children and infants.
If the airway becomes obstructed, the brain must bounce out of deep sleep and into a lighter stage of sleep in order to grind and clench to push the jaw forward to allow for breathing again.
Grinding and clenching are the body’s way of reopening a collapsed airway during sleep to start breathing again. This is why grinding and clenching are the new red flag for catching sleep apnea early on.
How Mouth Breathing Impacts Behavior and Personality
Interrupting deep sleep like this impacts development.
 Deep sleep is when Human Growth Hormone (HGH) is released, which is essential to a child’s brain development and long bone growth. Once deep sleep is interrupted, HGH stops being secreted. Not having enough HGH stunts your growth and brain development.
Deep sleep is when Human Growth Hormone (HGH) is released, which is essential to a child’s brain development and long bone growth. Once deep sleep is interrupted, HGH stops being secreted. Not having enough HGH stunts your growth and brain development.
Deep sleep is the body’s chance to restore, repair, and heal from the stress of the day. It’s a time of memory consolidation and cementing learning. Hormones that control appetite and other critical functions are regulated and stabilized during this stage.
In a child who is snoring, grinding and clenching, or breathing through the mouth, the brain is not able to rest and sleep is not restorative.
Children who are deprived of deep sleep are often hyperactive as a result of adrenaline used to compensate for sleepiness. They often aren’t able to achieve their academic potential because their brains and bodies aren’t at their best in this damaged, deep sleep-deprived state. They’re often diagnosed with ADHD and other behavioral issues. They have lowered immune systems, poor health, and can be overweight.
For more, check out my #1 bestselling book The 8-Hour Sleep Paradox.
Strategies for Parents
- Make sure your child can breathe through her nose with ease.
- Make sure your child has seen a dentist by age one. Make sure that this dentist is concerned with recognizing mouth breathing and its implications.
- Make sure your child is treated for allergies. Allergies can force children into mouth breathing.
- Make sure that your child’s diet and environment aren’t contributing to allergies.
- Ask your dentist if your child needs a referral to an orthodontist if he’s mouth breathing.

 C-Reactive Protein Testing: Why We Need Collaboration in Medicine & Dentistry
C-Reactive Protein Testing: Why We Need Collaboration in Medicine & Dentistry